As a physical therapist, I’m often one of the few healthcare practitioners that my clients spend more than 7 minutes with during an appointment.
This means I field a lot of questions they didn’t have a chance to ask their neurologist at their last appointment, including quite a few about Parkinson’s and Dyskinesia.
Below are a list of questions I often hear from my clients and our online community and my very best answers based on the most up-to-date research available. I’ve cited experts and research when I’m able to so you can find more information as you need it.
Please note: This article should not be taken as medical advice, only as helpful resources for you to use and share with your own healthcare team. I highly recommend discussing these topics with your Movement Disorder Specialist (MDS) or Parkinson’s neurologist before making any changes to your treatment regimen.
You can find an MDS in your area using this tool from the Parkinson Foundation.
What does dyskinesia look like in Parkinson’s?
Dyskinesia: Abnormality or Impairment of Voluntary movements.
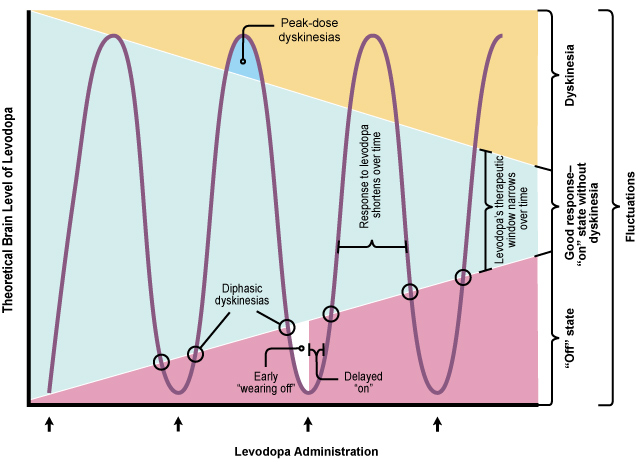
When your dyskinesia is fluctuating, it often falls into one of the following 4 patterns. Identifying which pattern your symptoms are most consistent with will help you and your neurologist decide on the best course of action going forward. Often times they can be addressed via adjustments to your DBS or medication dosages.
Peak Dose Dyskinesia
DEFINITION: Dyskinesia that increases during the time when your medication reaches its peak, right above your “optimal zone”. You have slightly more dopamine than you need and you become dyskinetic, and it starts to fade as you come back down into your optimal zone. These dyskinesias are often exaggerated by stress/anxiety and occur during other voluntary movements.
Two forms of Peak-Dose Dyskinesia you may not be aware of:
Ocular (Eye) dyskinesia - Upward gaze or “to and fro” pattern
Respiratory (Breathing) dyskinesia - Tachypnea (fast breathing) with irregular rate and depth
Diphasic Dyskinesia
DEFINITION: Dyskinesia that is present at the beginning and/or end of your medication dosage when l-dopa levels are changing from “off” to “on”, or from “on” to “off”, or both.
One form of diphasic dyskinesia you may not be aware of:
“Silly walks” - This is characterized by stepping with kicks, ballistic stamping with one of the legs, or high knee elevation when walking. It’s most common with YOPD.
Treatment options In the research: Bilateral STN Deep Brain Stimulation (DBS) markedly improved diphasic dyskinesia in 6 patients (2012).
Low-dose Dyskinesia
DEFINITION: This type of dyskinesia occurs during your “off” period. Typically this occurs early in the morning when you’ve been sleeping and are not fully medicated.
Stimulation-induced Dyskinesia
DEFINITION: This type of dyskinesia can occur in the early stage after STN Deep Brain Stimulation and is predominantly in one or both legs.
How do you Treat / Reduce / Control dyskinesia?
There are a variety of approaches you can use to help with the management of Peak-Dose Dyskinesias:
#1. Reducing your L-dopa dosages
Adjusting your medications so you spend more time in your “optimal zone” is one of the first strategies your neurologist will use to bring your dyskinesias under control. (Please only adjust your medication under the supervision of your healthcare team.)
#2. Amantadine
Amantadine is the only drug currently approved for its antidyskinetic properties and it does appear to have some long-term efficacy. However, studies have not extended beyond 12 months.
The newer Extended Release (ER) formulation of Amantadine was also shown to increase "ON" time without troublesome dyskinesia and reduce "OFF" time in a 2016 study. However, adverse effects were very common (occurring in 80-95% of patients) and included constipation, hallucinations, dizziness, and dry mouth.
#3. Other Medication “newbies”
There are some other "newbies" on the block when it comes to dyskinesia. Here's what we know from the research:
Studies regarding the impact of cholinergic drugs is ongoing.
Eltoprazine (7.5mg) was found to reduce Clinical Dyskinesia Rating Scale scores.
Safinamide has had mixed results extending "ON" time without troublesome dyskinesias.
#4. Device-aided Therapies
Due to the dysfunction of the gut and intestinal tract in those with a Parkinson's diagnosis, options for non-oral treatments are in high demand and the research on these options are growing. Here's what we know about non-oral options for dyskinesia so far:
Deep Brain Stimulation (at the STN or GPI locations in the brain) has been shown to help with the management of dyskinesias.
L-dopa intrajejunal infusions have been shown to decrease "OFF" time.
Sub-cutaneous apomorphine has been shown to increase "ON" time.
What Causes Dyskinesia in Parkinson’s?
Is there a correlation between longtime use of carbidopa/levodopa medications and onset of dyskinesia?
Motor complications such as dyskinesias very commonly increase over time after a diagnosis of Parkinson’s due to increasing dopaminergic treatment dosages over a long period of time. However, the degree of progression varies from person to person and there are a lot of strategies you can use to minimize your risk and prevent dyskinesia in the long-run.
First, a term you should know: Levodopa Induced Dyskinesia (LID)
LID explains why use of levodopa causes dyskinesia over time.
What is illustrated on the graph above, is that over time the amount of l-dopa you’re producing is decreasing, so it takes higher dosages of l-dopa to get up to functional levels (ie. out of the purple “low” zone and into the blue “optimal” zone).
As your medication dosages increase, you’re at a higher risk of developing LID.
For those of you who like to dive into the research and medical jargon, here is an excerpt from a study published in Postgraduate Medical Journal that explains the possible causes of LID*:
“Despite significant advances, the pathogenesis of LID remains incompletely understood. It is known that dyskinesias appear only after dopaminergic therapy and there is a time lag between the start of treatment and the emergence of LID.
Several possible mechanisms, both peripheral and central, have been proposed. They include reduced buffering capacity of the remaining intact neurons, dietary proteins, role of D3 receptors, and the role of glutamate receptors. While dietary proteins and gastric absorption have some relevance in producing fluctuations and “wearing off” associated with chronic levodopa therapy, central mechanisms are of greater importance for the genesis of LID.
It is suggested that pulsatile (as opposed to a continuous, physiological) stimulation of the postsynaptic receptors due to intermittent administration of levodopa leads to downstream changes in proteins and genes, causing alterations in striatal output in a way that promotes dyskinesias.”
3 Factors that Increase your Risk for Motor Complications in the Long-run:
Younger age at onset - When you’re diagnosed at a younger age, you’re going to be taking medications for a longer period of time.
Lower Weight - The theory here is that there are increased serum concentration of l-dopa in your system relative to your body weight and, thus, potentially more potent in your system over time.
Female Gender - This is thought to be due to hormonal differences between men and women.
So, now that you’re aware of the risks of developing motor complications like dyskinesia over time, let’s move onto some proactive strategies you can use to minimize your risk as much as possible.
How to Avoid Dyskinesia
There are three prevention strategies - one pharmacutical, two non-pharmacutical - you can use to stack the cards in your favor against dyskinesia in the long-run.
#1. Use of Dopamine Agonists
Dopamine agonists favored in younger patients have been shown to reduce dyskinesia and motor fluctuations. However, they do increase the risk of developing Impulse Control Disorders, somnolence and sleep attacks which can impact overall quality of life.
#2. Exercise Regularly for Neuroprotection
The best way for you to minimize the amount of medication you’ll need to take over time is to be exercising regularly. Exercise significantly increases the effectiveness of the dopamine you have in your system so you can take less medication overall.
Learn More about Invigorate’s online Parkinson’s-Specific Exercise Program
#3. Fight Constipation with Fiber & Fluids
When you take your medication orally, it has to be absorbed through your gut. If your system is backed up and not moving optimally, you’re likely not going to absorb your medication properly.
Less absorption = Higher dosages to get the same results.
Work to optimize your diet with whole foods that are high in fiber (like vegetables, nuts, seeds, and sprouted grains) and stay hydrated.
Is Physical Therapy Helpful for Dyskinesia?
When it comes to directly controlling dyskinesias, physical therapy is most effective when used in combination with other treatments like medication and DBS.
A skilled physical therapist can help you strengthen specific weak muscles that will improve your coordination and balance.
More importantly, a Parkinson’s PT can help you build a comprehensive exercise program that’s specific to your Parkinson’s symptoms and is best suited to keep you active and mobile for the long-run.
Find a Parkinson’s Physical Therapist near you:
Do you have a Parkinson's Plan of Attack?
Most people don't. Snag your free Plan of Attack Foundations PDF Checklist to start re-defining your diagnosis.