Raise your hand if you’ve ever had this thought:
“I could do all the things I need to do for my Parkinson’s symptoms, if only I had more energy!”
If you don’t have your hand up, it’s probably because you don’t have the energy.
Exhaustion and fatigue are some of the most challenging Parkinson's symptoms - alongside apathy and lack of motivation - to pinpoint and improve.
Today I want to walk you through 5 areas you can investigate to help you determine what may be draining your energy, along with ways you can upgrade in order to get some energy and vigor back into your daily life.
Here are the 5 Areas we’re going to dive into:
#1: Movement
#2: Sleep
#3: Blood Pressure
#4: Nutrition
#5: Social Health
Before we get started, remember that this is just general advice. You should be discussing all of your issues with energy and fatigue with your healthcare team so they can tailor all of this information to your specific situation.
Prefer to watch the video?
Video Breakdown
4:35 - Area #1: Movement
8:22 - Area #2: Sleep
17:31 - Area #3: Blood Pressure
22:57 - Area #4: Nutrition
27:48 - Area #5: Social Health
Area #1: MOVEMENT
Movement - my favorite topic!
When you're not actively using your heart, your lungs, and your muscles to move fluid around your body, it sits inside you like water in a stagnant pond.
On the flip side, when you’re moving around - exercising and being active - your body’s fluids are moving around like a river, rushing from one point to another. As you move fluid around, you also push nutrients to your organs, flush out toxins, and help your body heal.
This brings fresh life and fresh energy to your entire being.
Get up and move first thing in the morning, if you can.
It can be tough to get moving first thing in the morning, so start with a basic stretching routine like this one from our online exercise program. As you gently introduce movement, you’ll notice your energy start to perk up.
Start gentle, then slowly increase your intensity for a minimum of 10 minutes.
Stretching is wonderful, but exercise works best when you raise the intensity and your heart rate.
Start with 10 minutes. Set a timer. Tell yourself, “I don’t have to enjoy this 10 minutes, but I’m committed to following through.” If you finish 10 minutes and still want to quit, then you can. On the other hand, if you’re feeling good, see if you can add 5 more minutes.
Add on extra time slowly and soon you’ll be able to workout for 30, 45, or even 60 minutes. It takes time to build endurance, and the important part is to do a little more today than you did yesterday.
Give your new program 3 weeks to kick in. Most people require some time to adjust, but as you become more active, you’ll likely notice you have more endurance throughout the day and your feelings of fatigue will start to lift.
Need help getting moving? Want to work out on your own schedule? Click here to learn more about our online Parkinson's exercise program, The Booster.
Area #2: SLEEP
This area can seem a bit obvious..
You’re tired? You’re probably not sleeping right!
However, there are some Parkinson’s specific challenges you should be aware of on your quest to improve your sleep.
Optimizing your sleep routine = Priority Numero Uno.
The answer is not in a sleeping pill.
Don’t get me wrong - I think medications can be wonderful tools. However, throwing a Xanax or an Ambien on top of a terrible sleep routine will only cause more problems down the road, including grogginess and balance issues in the daytime.
For a deep-dive into how to get your nightime routine dialed in, check out this blog post:
How to Optimize Your Parkinson’s Sleep Routine
Some of the most important things:
Create a schedule and stick to a consistent bedtime and wake time, no matter what, for 3 weeks.
Reduce blue light exposure (from TVs, computers, phones, and tablets) after sundown
Wind down with journaling, meditation, deep breathing, or other mind-calming activities
Once you have a routine in order, you can check out a few awesome products I recommend as part of a “Parkinson’s Sleep Kit” that can help you go a little deeper (including a styin’ pair of glasses and a nighttime drink) here:
Parkinson’s Sleep Kit: 5 Products to Help You Seize those ZZZs
if you’re still having trouble sleeping after you’ve optimized your routine, it’s time to pull out the big guns.
It may be time to get checked for a sleep disorder.
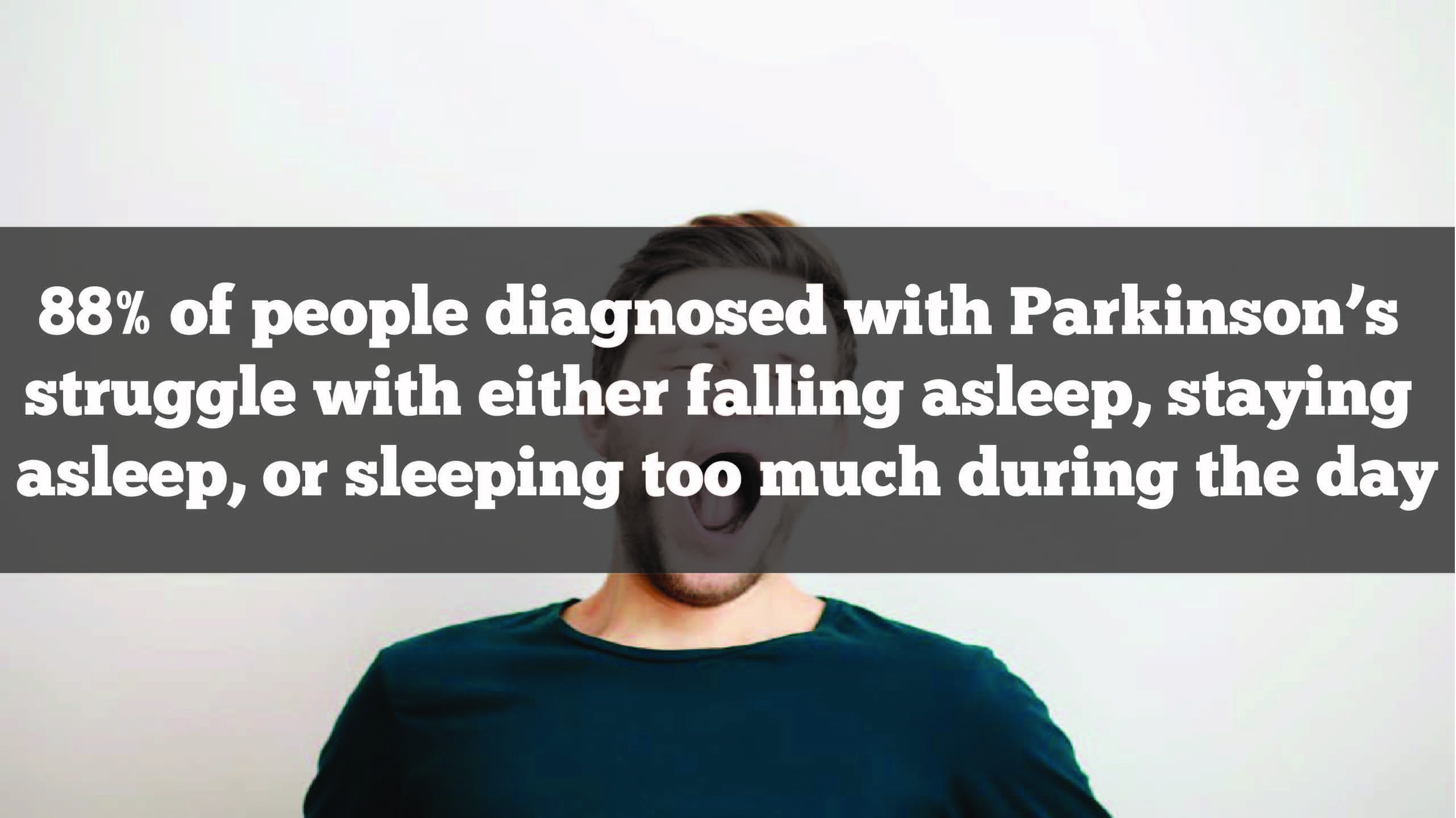
There are 3 disorders commonly seen in the Parkinson’s community, each of which can be tested for and addressed.
These disorders can contribute to Excessive Daytime Sleepiness (EDS) which is a state where you feel incredibly groggy throughout the day, may take multiple naps during the day, and continue to feel extremely fatigued despite a regular exercise routine.
Sleep disorders that are common in Parkinson’s:
Insomnia - Difficulty falling asleep OR difficulty staying asleep,
REM sleep disorder - When your body doesn't completely paralyze itself as you're sleeping and so you end up acting out your dreams physically.
Sleep Apnea - you’re not getting enough oxygen at night due to breathing obstruction
Reporting any symptoms you’re having around sleep, including ones associated with these 3 sleep disorders, is important so your physician can start helping you investigate and treat your sleep challenges.
Area #3: BLOOD PRESSURE
Out of sight, out of mind.
Such as it is with blood pressure.
If you’re chronically fatigued or exhausted, and not tracking your blood pressure regularly, you could be missing a huge piece of the energy puzzle.
American Heart Association: How to Track Your Blood Pressure
If you feel woozy, exhausted, fatigued, heavy, or lightheaded you may be combating Orthostatic Hypotension (OH).
OH is a sudden drop in blood pressure when you change positions due to blood rushing away from your head into your extremities. It typically occurs while going from laying down to sitting up, or sitting to standing. It can contribute to falls and may happen after meals (called “post-prandial” hypotension) when all the blood is rushing to your digestive system.
If this is you, consider slowly changing position, staying hydrated, and wearing compression stockings to keep blood from pooling in your legs.
When your blood pressure is chronically low, you can have reduced blood flow to your organs and brain - something called Chronic Hypoperfusion.
It’s no surprise that this can make you feel drained.
While hypoperfusion takes a multi-faceted approach, the very best thing you can be doing is staying properly hydrated so your blood pressure stays elevated and within normal limits.
For more strategies on how to stay hydrated, beyond simply drinking more water, check out this post:
Staying Hydrated with Parkinsons: Going Beyond “Drink More Water”
No matter what your issue is, if you’re not hydrated you’re making everything worse!
Area #4: NUTRITION
When you put diesel fuel into a gas car, it’ll run for a while. However, eventually your engine is going to stop running and you’re likely going to incur some damage to the engine.
The same is true with your body.
When it comes to your energy levels, it’s important to remember that you’re just a bunch of cells. Your cells need nutrients to function properly. When you’re not fueling your cells, you feel it.
This is where proper nutrition comes into play. It’s not just about calories-in versus calories-out. It’s about the quality of the food - the fuel - you’re putting into your system.
Nutrition for Parkinson’s and brain health is a massive topic in and of itself. I cover it extensively in a free 4-part video series that you can access here:
Access the Parkinson’s Gut Health Video Series (+ Free PDF Workbook) Here
As a general starting point, it’s crucial for you to avoid foods that will “gunk you up.”
These include:
Sugar in all of its processed forms (soda, juice, and Splenda included!)
Processed foods (cookies, cakes, pastries, sugary-cereals, etc)
Fried foods
Unhealthy oils like vegetable oil and margarine
By no means is that list all-inclusive, but it’s a good start.
Start replacing them with fresh, fibrous, nutrient-dense foods like green vegetables, sprouted grains and lentils, healthy fats like olive oil and avocados, and wild-caught fish.
If you want to learn more about the low-down on gluten, sugar, wheat, dairy, and more - head over and watch the Parkinson’s Gut Health video series. It’ll answer all your questions, and then some!
I hear some of you saying, “What supplements should I take?”
I cover that in the video series, too, but please know this:
You can’t supplement away a bad diet. Period.
Area #5: SOCIAL HEALTH
In this disconnected world, human connection has become a crucial part of our health.
Research suggests that people who connect with others in a meaningful way and feel like they have a support system around them that they can trust live longer and say they have a fulfilling, happy life.
So, how often are you connecting with others?
When you’re not consistently seeing others, interacting with them, talking about your life and spending quality time with people you care about, it’s very common to slip into depression or apathy that can get confused with fatigue.
Do these sound like you..?
You lack interest, concern or enthusiasm. (This is Apathy.)
You feel a significant feeling of loss of hope, sadness, or low spirits, which is often paired with guilt or feelings of inadequacy. You lack energy and your sleep and appetite are both disrupted. (This is Depression.)
Seeing other people and feeling part of a tribe is crucial to boost your feel-good endorphins, mood, and energy.
Find time and ways to connect with people face-to-face.
Meet up for coffee, a walk, or a show. Go to church or a meditation center. Keep a weekly lunch date with a small group of friends… or whatever else floats your boat!
Before you say, “I don’t really need other people. I’m fine on my own.”, hear me when I say:
Connection is a nutrient, not a coping mechanism. You need it to survive.
Get out of the house and go somewhere. Even if it takes extra time, it’s worth doing and being consistent.
NOTE: It’s very normal to feel sad after a diagnosis of Parkinson’s, and it can turn into depression when you’re having a hard time processing your feelings and emotions. I highly encourage you to talk to a grief and loss counselor who can help you take the next healthy step.
Which area are you going to dive into first?
Let me know in the comments section below.